Reducing expensive OR schedule delays using QHealth’s RFID Workflow Optimization
Paula Dycaico, Director of Marketing at Quake Global
\Maintaining profitability for hospitals requires a complex calculation that combines the need for improved outcomes, improved quality, and favorable patient satisfaction scores. At the same time reducing cost is a higher priority than ever before. Value-based care and bundled payments all contribute to reduced reimbursements that have resulted in smaller margins for hospitals.
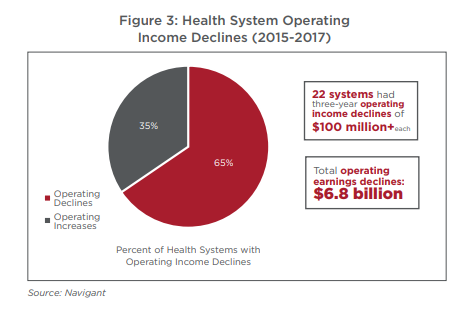
A Navigant survey published in 2018 found that U.S. hospitals and health systems experienced an average 39% reduction in their operating margins from 2015 to 2017 because their expenses grew faster than their revenues.
Navigant https://www.navigant.com/news/corporate-news/2018/hsom-analysis-2018
In the operating room and other procedural areas, reducing costs is especially critical due the high cost of care in those environments. Operating rooms are the most resource intensive part of the hospital per square foot and the staff resources are among the most highly paid.
In a study published in 2011,1 hospitalizations that involved operating room procedures constituted 29 percent of the total 38.6 million hospital stays in the United States and 48 percent of the total $387 billion in hospital costs. In addition, the study found that on average, hospital stays that involve an OR procedure have been reported to be 2.5 times costlier than stays that do not involve an OR procedure. In California, 1 minute of operating room (OR) time costs an average $36 to $37 per minute, according to a study published in JAMA Surgery.2
To remain in business and provide the best care for their patients, hospitals must scrutinize all expenses and ensure that any new process or products will result in a measurable ROI that pays for itself with efficiency or improved processes.
What are the most common problems that generate the most revenue leakage?
According to a study published in NCBI/NIH. Delays in procedure start times represent the most common type of problem in the OR and more than half of all cases had at least one delay.3 A delay in the first case of the day will impact subsequent procedures which creates a ripple effect across the entire day's schedule.
What causes delays?
One of the biggest challenges is unpredictable patient behavior. Patients who arrive late or cancel at the last minute can create significant scheduling bottlenecks. In addition, everything from inaccurate scheduling per procedure type, room turnover time and patient, staff and equipment availability can impact the cost of procedures. Some elements are unpredictable, such as an unexpected complication during a procedure that extends the planned OR scheduled time. In the end, while hospitals can’t plan around the unpredictable, they can improve process problems that occur regularly in the clinical environment.
When valuable clinical resources get delayed or interrupted with administrative tasks, such as managing a delayed schedule or finding a missing patient, costs increase and revenue decreases. The impact to the schedule is felt across multiple functional areas that represent high dollar resources, such as surgeons, anesthesiologists, and surgical nursing staff. Every minute counts when the costs of a delay are so high.
Any delays can negatively affect the quality of care and can significantly impact patient satisfaction regarding their treatment experience which can reduce satisfaction scores. Lowered satisfaction score can negatively impact reimbursements, It’s a vicious cycle.
How can you fix the most common problems that cause delays?
Workflow optimization starts with the most important member of the hospital population, the patient. Using a passive RFID system for active and immediate visibility with Quake Global’s QHealth Enterprise system to locate patients from the moment the patient arrives in a facility to when they are discharged ensures the OR schedule can be kept on track. if the staff knows a patient has not arrived, they can adjust the schedule to start other procedures to ensure no staff or rooms are underutilized for the day and mitigate the risks of lost time and revenue. When the OR staff is confident about the location of patients, they can avoid wasting time finding patients and focus on providing high-quality clinical care.
How can QHealth help?
QHealth’s Passive RFID clinical workflow solution provides accurate visibility to each part of the puzzle that causes delays and allows enhanced process management based on true visibility, rather than on relying on manually reported location. With accurate real-time location, the clinical staff can reduce or eliminate scheduling gaps which will ensure workflows are efficient and care is delivered in a timely manner. The result of better visibility is lowered facility costs, increased revenue, efficient use of resources, better quality of care and increased patient satisfaction.
Over time, analyzing the data about OR utilization can allow facilities to continually optimize processes on an ongoing basis, monitor to ensure established processes are followed and identify new challenges with workflows. Using Quake predictive analytics can allow a facility to model and plan future workflow optimizations that offer ongoing value to process improvement initiatives.
QHealth Enterprise Solutions use RFID workflow optimization to provide synchronized simultaneous 360o visibility to everything that matters in healthcare with comprehensive data analytics that drive meaningful operational transformation.
1 Weiss AJ (Truven Health Analytics), Elixhauser A (AHRQ), Andrews RM (AHRQ). Characteristics of Operating Room Procedures in U.S. Hospitals, 2011. HCUP Statistical Brief #170. February 2014. Agency for Healthcare Research and Quality, Rockville, MD.
2 Childers CP1, Maggard-Gibbons M1. JAMA Surg. 2018 Apr 18;153(4):e176233. doi: 10.1001/jamasurg.2017.6233. Epub 2018 Apr 18. Understanding Costs of Care in the Operating Room.
3 Janice Wong, BS, MS, Kathleen Joy Khu, MD, Zul Kaderali, MD, and Mark Bernstein, MD, MHSc., Delays in the operating room: signs of an imperfect system, Can J Surg. 2010 Jun; 53(3): 189–195.


Comments (0)